Canadian Health Experts Speak Up About The Decision to Lockdown
Dealing with COVID-19: An open letter to Canada’s prime minister and provincial and territorial premiers
Dealing with COVID-19: A balanced response
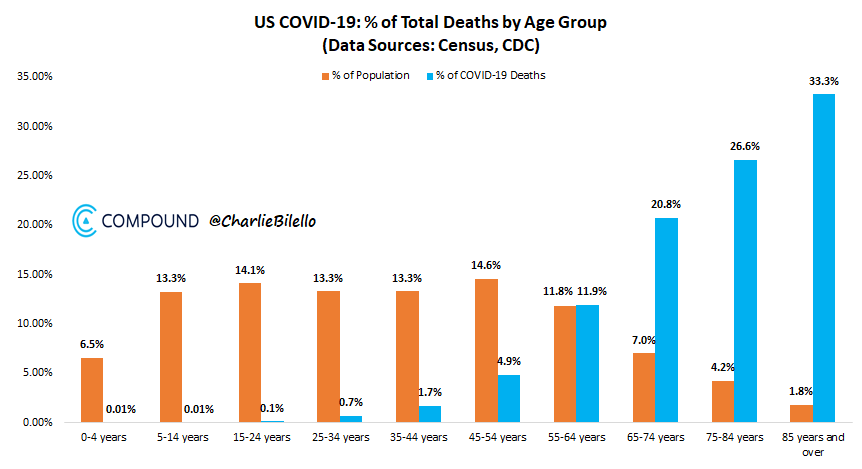
COVID-19 is a serious public health threat and will remain so until we have a universally available safe and effective vaccine or similar medical treatment. There have been many deaths due to COVID-19 and every single one represents a tragic outcome. However, in overall population health terms COVID-19’s direct impact on premature mortality is small. While those under the age of 60 account for 65 per cent of cases, they represent just three per cent of deaths. With ready access to health services, severe outcomes can be averted in those who do not have pre-existing risk factors.
In March 2020, unprecedented public health measures were implemented in Canada in response to the rapid rate of growth of cases and the potential threat to health system. Because of the potential for exponential growth in cases and the situation in other parts of the world, our governments took these actions that applied to the entire population to protect our healthcare system. These interventions were meant to buy the time necessary to develop a longer-term response. They should not be used as a means of eradicating the disease.
While some countries have been successful in suppressing the disease, most continue to see sporadic cases and outbreaks. Only a few countries, primarily island nations, appear to have eliminated the disease, but it is uncertain how long those countries can completely isolate themselves from the rest of the world.
The public health measures did protect our healthcare system, to the point that Canada had excess capacity. Our leaders and public health authorities had to use strong language to support universal acceptance of these measures. As a result, many Canadians have become fearful of COVID-19 and are worried about the impact of working, seeking routine and preventative medical care, participating in religious and cultural events, interacting with their family and friends, using public transportation, shopping and other normal activities.
COVID-19 control is an important public health priority but it is not the only or the most important challenge to the health of people in Canada. We need to examine the broad social determinants of health and their impact on citizens, particularly with an equity lens, as the consequences of the public health measures have not been shared equally in society. Those in lower income groups, Black and other racialized groups, recent immigrants and Indigenous people are bearing disproportionate burden. The public health efforts must take account of the impacts of both the disease and the consequences of the control measures on all segments of the population.
The fundamental determinants of health – education, employment, social connection and medical and dental care – must take priority. Measures for COVID-19 control need to accommodate these health determinants. Children need to interact with their peers in child care, schools, sports and social activities and summer camps. Adults need to go to work. Family and friends need to meet.
The societal costs of maintaining these public health measures, even with some gradual relaxation, are too high. Canadians are missing scheduled medical appointments and surgeries, which will lead to increased deaths. There are significant challenges for our young with impact on early childhood development, one of the strongest predictors of life-long health and social outcomes. Education is compromised. There are increases in domestic violence, alcohol and drug intake, and food insecurity.
The economic consequences are huge. This leads to increased unemployment, which is related to increased deaths. And the toll on mental health is just beginning to be felt. Personal concerns about the disease, cases and deaths in friends and family, loneliness and isolation, worries about jobs and finances, parents having to juggle childcare and general insecurity are leading to increased levels of anxiety, depression and stress.
We need to shift from a mindset of attempting to eradicate this disease, which is not feasible and will lead to continued devastation of our society, to a new goal.
Our new goal: Minimize the impact of COVID-19 using methods that are practical, effective and compatible with our values and sense of social justice. We need to focus on preventing deaths and serious illness by protecting the vulnerable while allowing society to function.
Elimination of COVID-19 is not a practical objective for Canada until we have a vaccine. We need to accept that there will be cases and outbreaks of COVID-19. We should mitigate the effects of the disease with measures that are equitable, sustainable and acceptable. This includes testing and contact tracing, and ensuring that health services with access to the latest treatments are available for those who contract the disease.
Those at highest risk of severe consequences need to be offered effective protection from COVID-19, particularly those in long-term care institutions, but this protection must be respectful of their autonomy and allow them a reasonable quality of life.
Aside from the outbreaks in long-term care institutions, some of the most significant have been in other congregate living settings (homeless shelters, prisons, dormitories for temporary foreign agriculture workers) and work settings such as meat-packing plants. Appropriate protections and supports are needed in such settings.
COVID-19 control must be balanced with basic human rights. People need to be empowered to make informed choices about their own lives and the level of risk they are prepared to accept. Universal public health measures are appropriate only when they are truly necessary, supported by strong evidence, and when there are no other alternatives.
Recommendations
1-Carefully reopen schools, businesses and health care. Allow gatherings of friends and family. Provide practical guidance that allows citizens and institutions to operate safely and effectively. Restore public confidence that it is safe to go out, that appropriate precautions are in place and conditions will be closely monitored.
2- Develop clear control plans for future outbreaks or resurgence of disease that are risk-based and focused so further universal lockdowns are not necessary.
3- Improve our disease surveillance so that we have an accurate picture of disease activity to make timely decisions and provide useful advice to Canadians. Ensure that public health has the resources to conduct timely and effective testing and contract tracing.
4- Provide clear guidance on appropriate use of viral (diagnostic) and antibody (serology) testing for healthcare providers, employers and community organizations. While testing is a critical element for control of COVID-19, it has to be done in a smart way. Indiscriminate testing, for example daily testing of all employees in an office setting, is less effective than testing of those with greater exposure to the general public.
5- Assess community risk in applying infection control approaches in different settings. Procedures that are appropriate for a hospital, with high risk of exposure, are not necessary across all of society. Control measures need to be evidence-based and address the level of risk in a particular setting and community. Measures should take account of costs and benefits at the individual and community level using a social-determinants-of-health model and applying an equity lens.
6- Assess the appropriateness of recommendations for physical distancing from a risk benefit perspective. Where risk of community transmission is very low, the absolute benefits of physical separation are negligible, particularly if good hygiene is practiced and individuals with symptoms stay home.
7- Reassess quarantine and isolation periods based on current evidence. Strategies that use testing to further reduce this period should be examined. Review the restrictions on nonessential travel to all parts of the world. Travel should be restarted to countries where there is little community transmission.
8- Be clear on when the use of medical and non-medical masks is recommended. When advice varies based on local epidemiology, provide clear evidence-based criteria for decision-making. Any requirements for mandatory masks must be based on strong evidence with clear specification of where they are most appropriate (close quarters, congregate living settings, etc).
9- Improve infection prevention and control in long-term care as deaths have come mainly from a break down in these practices within some facilities.
10- Canadians must be better informed about their true level of risk from COVID-19. An accurate accessible risk assessment tool is a priority. This will help empower people to make informed decisions about how they choose to lead their lives. Help people understand and manage their fear and anxiety.
11- Provide support for vulnerable people living in the community who choose to isolate when the disease is active. Some individuals, even though at risk for severe disease, may wish to make informed decisions to carry on with normal life. Such choices should be respected and supported.
12- Ensure there are adequate supports for those individuals that have been adversely affected by COVID-19, or the consequences of the public health measures. In particular, support for mental health and addictions is essential as the potential toll on the population is massive.
Source: Click to access site